A Severe Toothache
It may come and go but you should still be examined
Dear Doctor,
I had a tooth filled a few months ago. It was a big filling and my dentist warned me that the decay he removed was close to the nerve. The tooth was quite sensitive to hot and cold for a while. The tooth then became unbearably painful for a day or two then the pain just went away. Am I OK now?

Dear Regina,
I'm not so sure you're OK now, here's why. Deep decay in a tooth that is close to the nerve, or more accurately the “pulp” of a tooth (which contains nerve tissues), may well result in inflammation, called quite literally “pulpits.” This inflammation is not much different than any other type of inflammation which occurs in our bodies, except the pulp is in an enclosed space and has no room to swell up. This hinders its capacity to heal on its own.
The temperature sensitivity you noted at first was probably the result of a low grade inflammation which resulted from the removal of the decay. Decay contains bacteria which must be removed to stop caries, the decay process, from progressing. If the decay is too close to the pulp it may be too late to stop the pulp from becoming infected and hence inflamed. This may be felt first as temperature sensitivity, but if the defenses of the pulp become overwhelmed, it dies. This is felt as severe or acute pain that typically lasts for a day or two. Then the pain actually goes away, because the nerves that transmitted the pain die along with the pulp tissue. The good news — no more pain; the bad news — it is the beginning of an infection, which can become quite chronic; i.e. slowly progressive and painless, until at some time in the future when it too can become acute and cause a painful abscess.
The only way to know which outcome occurred in your case is to have a dentist test your tooth.
Having said this, there is also a chance, although rather minor, that the pain rapidly goes away because the nerve spontaneously heals. So the most accurate answer to your question is that what happened depends upon the extent of the decay and how the pulp of the tooth has responded.
The only way to know which outcome occurred in your case is to have a dentist test your tooth. Given your story, it is more likely that the nerve (pulp) has died and therefore the tooth's vitality (whether the nerve is still living or not) should be checked. This can be done very simply by testing the tooth to see if it responds to temperature, usually by the application of some ice to the tooth or other simple means.
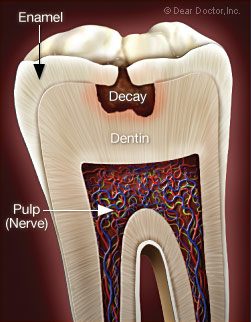 |
| Illustration showing the decay close to the pulpal (nerve) tissue. This has the potential to cause pain. |
If in fact the nerve is non-vital (the pulp tissue has died), root canal or endodontic treatment (endo – inside, dont – tooth) will be necessary. This is an everyday procedure in dentistry in which a small “access” cavity is opened from the top of the tooth to gain access to the pulp “chamber,” the part of the tooth that houses the pulp. This allows for the dead pulpal tissue to be removed, the root canals to be cleaned, disinfected and prepared for a filling which seals the canals and thereby prevents further infection. Importantly, once the pulp and the nerve tissue it contains are no longer living, root canal treatment is almost completely pain free.
While simple root canal or endodontic treatment can be carried out by a competent general dentist, it is a speciality area of dentistry. Optimal endodontic treatment requires proficiency in the use of microscopes. An endodontist is a specialist in this area of dentistry who has taken advanced training in the diagnosis and treatment of these kinds of problems. Many general dentists perform root canal treatment procedures, but may defer complex cases to an endodontist. Your dentist will advise you about the status of the tooth and will refer you to an endodontist if necessary. Once endodontic treatment is completed, most teeth require a cap or crown in order to protect the tooth from fracture. This would be made by your general dentist.
So to truly find out what has happened and answer your question, you would need to be re-evaluated by your dentist or an endodontist who can properly diagnose what has happened and provide the appropriate treatment.




