Infections Around Dental Implants
Food below the gums can cause infection
 Dear Doctor,
Dear Doctor,
I've had a crown supported by an implant for several years, but recently the gum around it has become inflamed and swollen. I recently got a popcorn husk stuck inside the gums and they've been inflamed ever since. What should I do?
Dear Allison,
Food collecting around teeth and implants is not uncommon. And unquestionably some areas collect more food than others; that has a lot to do with “local anatomy,” a fancy way of saying the local shape and position of the teeth relative to one another. If the teeth are not perfectly aligned with normal tight contact relationships, food material is not deflected away from the gum tissues effectively. Therefore, it collects causing stagnation, or more damaging, food impaction may occur.
Occasionally certain types of food, classically popcorn husks or kernels, tiny seeds and the like, can get caught between the soft gum tissues and the teeth or implants to which they are attached. Like small sharp razors, they can sever the attachment causing the gum to become inflamed, and if these food particles are not removed the gum tissues subsequently become infected.
Impaction of food, the forceful wedging of food or other foreign materials between the gum tissues and teeth, or implants can be more serious. It causes a similar but generally more noticeable inflammation and/or infection. It is simply more painful, and worse still when biting — more material can be forced into the space.
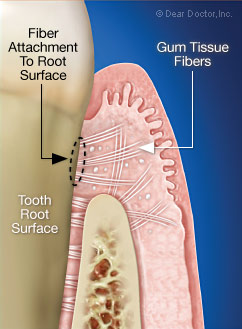 |
| Note how the gum tissue fibers are attached to the tooth root surface. |
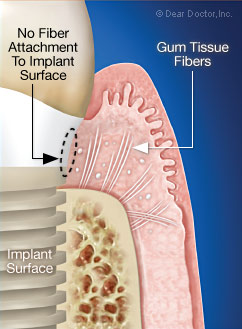 |
| Note that there is no fiber attachment to the implant surface. Instead, there is a tight tissue adhesion. |
Tissue Attachment — Teeth Versus Implants
A quick understanding of the nature of the attachment of the gum or gingival tissues to the teeth and in your case implant, will be useful so that you can understand why in fact implants are a little more vulnerable once an inflammatory process is set up. Both implants and teeth are stabilized and connected to the bone from which they derive their support, but at the gum level, at the very top, the epithelial layer of cells (“epi” – top or covering; “thelial” – layer), directly contact and connect to both implants and teeth in a very interesting way. They actually stick to the surface of the implants and the teeth.
Under a high power microscope they look like little rows of suction cups. The cells themselves are connected in specialized areas by similar suction like-structures running from cell to cell (called desmosomes), and from gum to implant or tooth surface by hemi-desmosomes (“hemi” – half).
The other significant difference between the gum tissue attachment to teeth is the fiber arrangement in the connective tissue, which attaches directly into and around the teeth. These fibers are continuous with the periodontal ligament (“peri” – around; “odont” – tooth), which also join the teeth to the bone. The counterpart of these fibers in the implant situation is that they run behind and beneath the epithelial cells, thus helping to form part of a tight tissue adhesion.
But it's not just the nature of the attachment to the tooth; it's also the type of tissue that buffers wear and tear at the gum level. The surface tissue around the teeth naturally contains a protein called keratin, which imparts toughness to the tissue, making it stiff, inflexible and wear resistant. Together with the underlying connective tissue into which it is anchored, this toughness really does make gum tissue very resistant to wear and tear. It is generally acknowledged to be important around implants as well as teeth.
The Significant Difference
Healthy gum tissues, kept free of inflammation by daily removal of bacterial plaque biofilm, brushing and flossing, are generally quite resistant to the invasion of bacteria, or mechanical trauma caused by abrasive foods. If bacterial plaque biofilm is allowed to accumulate, the gingival tissues will become inflamed, and the epithelial lining cells that connect to the teeth will become unglued for want of a better word. In fact, they unzip from the implant or tooth surface, losing their tight attachment and allow foreign material to penetrate into the space formed.
Inflamed tissue is less resistant to bacteria or food particles entering into the space created. Thus a vicious cycle is set up; once the normally tight gum tissue attachment is lost and material is trapped inside, bacteria and their harmful by-products have the potential to destroy tissue and bone beyond repair. It is generally, but not always possible to remove bacteria and trapped foreign material without professional help.
Some medical conditions e.g. diabetes and smoking can make the problem worse. If an acute infection occurs like an abscess, it has the ability to rapidly destroy the implant bone connection. This is known as peri-implantitis, (“peri” – around; “implantitis” – inflammation of the tissues surrounding implants). This can be serious because in a healthy state the bone is fused or integrated into the implant surface, but when infected this union “dis-integrates,” and over time, may lead to implant loss.
What To Do
As with all health issues, the best thing to do is to see your dental health professional for a proper assessment and diagnosis of the situation.
Treatment will be based on the degree of inflammation, infection and damage to the gum tissues or implant. The most usual occurrence will be to first treat the inflammation and infection, usually by cleaning the affected area (with local anesthesia to numb it if necessary), irrigate with disinfecting solutions, and possibly antibiotics.
It is important to be seen as soon as possible to make sure that the implant surface has not become exposed and/or damaged. This eventuality may be difficult to treat; once an implant surface has become contaminated it is very difficult, if not impossible to get bone to reattach to it.
How To Help Avoid Problems
Implant maintenance is not only the responsibility of the dentist or hygienist but you, the patient as well. The long-term health and success of dental implants depends largely on your ability to keep them free of bacterial biofilm. A routine hygiene schedule is extremely important so that your overall dental health can be monitored. Your dental professionals will make recommendations and demonstrate personal oral hygiene techniques and the products and that will suit your individual needs.
This may be more than you wanted to know, but this is an important and not uncommon problem. Thank you for bringing it to our attention. I hope this information helps.





