HIV-AIDS and Oral Health
Appropriate Care Can Improve Quality of Life
 |
Today, some 35 million people worldwide are living with HIV infection — including about 1.2 million Americans — and about 50,000 new cases are diagnosed in the U.S. each year. Thanks to modern antiretroviral drugs, a large number of them will be able to manage the disease effectively, and enjoy a nearly normal lifespan. Many, however, will develop potentially serious oral conditions that are related to AIDS. Sometimes these are the first symptoms of the malady, and other times they indicate a change in the disease’s progress. That’s why it is critically important for HIV-positive patients to maintain good oral hygiene and receive regular dental care.
What Is HIV/AIDS?
HIV stands for human immunodeficiency virus. This is the virus that can lead to acquired immunodeficiency syndrome, or AIDS. It belongs to a class of retroviruses, pathogens that have a genetic blueprint and replication system that is different from most other viruses.
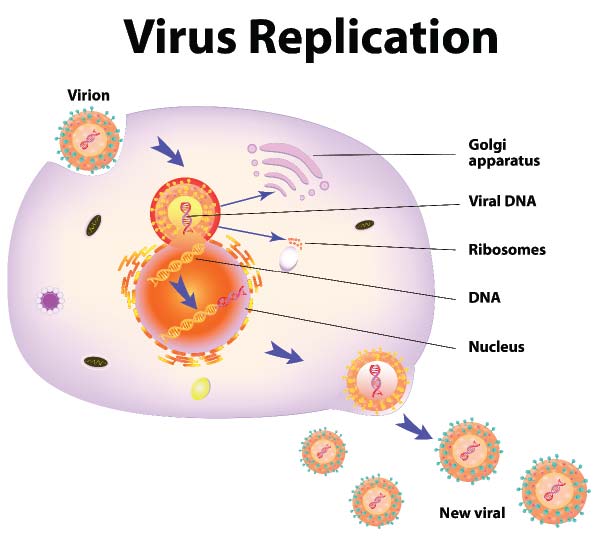 |
| When an individual virus (virion) is taken into a cell, it hijacks the cell’s replication system and causes it to make more copies of the virus. |
HIV affects specific cells of the immune system, called CD4 cells and helper T cells. These cells play a critical role in combating infectious diseases. If left untreated, HIV eventually destroys many of these cells — and without them, the body can’t fight off systemic and oral infections and other diseases. When this happens, HIV infection leads to AIDS.
Unlike most other viruses, the human body cannot get rid of HIV. That means that once you have HIV, you have it for life. Presently, there is not a cure for HIV/AIDS, although a great deal of research continues trying to find one.
Treatment for HIV is called combination antiretroviral therapy (ART). The medications used in ART can dramatically prolong the lives of many people infected with HIV and significantly lower their chance of infecting others. Before the introduction of ART in the mid-1990s, the vast majority of people with HIV progressed to AIDS in just a few years.
A Mysterious Malady
Today, scientists and medical researchers have learned a good deal about HIV and AIDS. Not so long ago, however, that wasn’t the case. When this malady emerged in the early 1980s, it caused so much fear and confusion that some likened it to a plague. At first, its effects were seen mostly on those whom society marginalized: sexually active gay men and injection drug users. Later, it was realized that this disease was global in scope, with the potential to affect anyone, anywhere.
One of the earliest goals in AIDS research was to identify and understand how HIV acts — and how people become exposed to it. It soon became clear that HIV spreads by contact with bodily fluids — particularly semen, blood, vaginal fluids, and breast milk. But it is important to point out that HIV is NOT spread by saliva, sweat, tears, feces or urine.
Researchers soon learned that HIV targets immune system cells, hijacking their cellular machinery to make more copies of the virus. This disables the body’s natural defense system, leaving it vulnerable to attack from a number of opportunistic infections. The later stage of infection, with well-defined clinical signs, is called AIDS. The disease is called a syndrome because it is a collection of symptoms that point to a complex illness, which can cause many different problems in the body.
The Oral Cavity Connection
What does all this have to do with the area dentists are most concerned with: the mouth? Perhaps surprisingly, the answer is: plenty. The oral cavity is often the place where the outside world first contacts the tissues of the body. It’s intimately involved with our senses of smell, taste and touch. Many times, it is the body’s first line of defense against disease — for example, healthy saliva plays an important role in helping our immune system fight infection. However, the mouth is also the place where many of the symptoms and conditions related to AIDS begin showing themselves.
In the early 1980s, dentists began seeing patients with symptoms in the mouth that they didn’t understand, and immediately realized these symptoms were connected to a more serious disease. Dentists were in fact among the first to recognize the symptoms that might indicate an individual had AIDS.
Today, antiretroviral therapy is helping to keep many people infected with HIV from progressing to AIDS. But when oral diseases are discovered in HIV-positive (infected) individuals, it may indicate a possible progression to AIDS associated disease.
HIV-Related Oral Conditions
It is estimated that 30-80 percent of people infected with HIV will develop oral problems. None of these diseases by themselves indicate that a person is HIV positive or has AIDS; however, if they are noted during a routine dental visit, and if the individual could potentially have come into contact with the virus, then a dentist might suggest testing to rule out the possibility of HIV infection. More often, these conditions are seen in people with various stages of HIV-related disease. Unfortunately, many people living with HIV/AIDS don’t get all the treatment they need for these issues, even though it could help them live longer and have a better quality of life.
 |
| Candidiasis (also known as “thrush”) is the most common oral condition associated with HIV. This fungal infection may appear as white patches on the tongue. |
Candidiasis (a fungal infection also known as “thrush”) is the most common oral condition seen in association with HIV infection. It may appear as a cracking or fissuring of the corners of the mouth; red, flat subtle lesions that most commonly occur on the top of the tongue and the roof of the mouth; or creamy white patches found anywhere in the oral cavity that can be wiped away leaving a red or bleeding surface.
Some other common HIV-related oral problems include: Xerostomia (“xero” – dry; “stomia” – mouth), a condition resulting from the lack of saliva; Kaposi’s sarcoma, a cancerous tumor that develops from the cells that line lymph or blood vessels; and Oral Hairy Leukoplakia, (“leuko” – white: “plakia” – patch) a virus that causes lesions on the surface of the tongue.
 |
| HIV-positive individuals are at risk for developing a severe form of periodontal (gum) disease known as Necrotizing Ulcerative Periodontitis (NUP). |
Periodontal disease is common in the general population — but there is a severe form that is sometimes found in people with HIV disease. This condition, known as Necrotizing Ulcerative Periodontitis (NUP), is a marker of severe immune deterioration. Often characterized by spontaneous bleeding of the gingival (gum) tissues, NUP causes ulcerations of the gums and a distinct and disagreeable odor. It may also be associated with significant pain, and in later stages loosening and loss of teeth. It’s possible to manage this condition with antibiotics, chlorhexidine mouthrinses, professional deep cleaning, and pain relievers. Individuals who have NUP should also be referred to their primary care providers for diagnosis and management of associated general or systemic AIDS.
What Should HIV-Positive Individuals Do?
By now, most people know the common risk factors for contracting HIV: having unprotected sex with someone who is HIV-positive, or coming into contact with needles, blood or bodily fluids that may contain the virus. Confidential testing is also widely available — you can input your zip code to find a testing location near you at the following URL: http://hivtest.cdc.gov. What many don’t know is that HIV-positive individuals need to be especially careful about maintaining excellent oral health — and they need to receive comprehensive dental care.
There are several reasons why proper dental and periodontal care is so important for people coping with HIV/AIDS. One is that regular oral health exams allow healthcare providers to monitor the progression of an individual’s HIV infection, and ensure that appropriate treatment is provided — for the benefit of the patient’s overall health, as well as the management of any oral issues related to HIV or AIDS. In fact, the sudden appearance of some oral diseases can indicate the onset of a more advanced stage of HIV/AIDS; others may indicate a change in an individual’s viral load.
Proper treatment can also help relieve many oral problems that may cause individuals to suffer discomfort and a reduced quality of life — for example, mouth sores, bleeding gums or loosening teeth. Pain management may also be an important factor in controlling the oral manifestations of this condition. Timely treatment can prevent more serious problems (such as severe periodontal disease) from developing.
While there is presently no cure for AIDS, most individuals with HIV are now able to manage the disease effectively. With appropriate ongoing treatment, many are able to lead much longer and healthier lives. Proper dental care should be recognized as an essential part of HIV/AIDS treatment. Regular exams and appropriate treatment for HIV-positive individuals are vital — not only to manage oral diseases and improve the quality of life, but also to provide important diagnostic information that reflects on an individual’s overall health.




