Gum Disease & Systemic Health
What's the connection between your oral health and general health?
 |
Can you name the number one cause of tooth loss in adults? It's not decay, accidents or teeth grinding. Instead, the culprit is periodontal (gum) disease—a "silent" malady that affects around one in two adults, yet often isn't recognized until it has progressed to a serious stage. But tooth loss isn't the only consequence of periodontal disease: It is linked to diabetes, heart disease and other so-called systemic disorders—that is, diseases that affect the entire body rather than just one organ or body part.
According to the U.S. Centers for Disease Control and Prevention, periodontal disease affects nearly half of all adults over 30, and 70% of those aged 65 and older. Around 64.7 million Americans have the more severe form of gum disease known as periodontitis. This oral infection can break down the gums and underlying bone, causing teeth to become loose or even fall out.
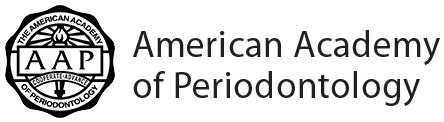
People who have periodontal disease often find it causes health problems that go beyond the mouth. Through years of research, scientists have established links between uncontrolled gum disease and serious health conditions such as diabetes, cardiovascular disease, Alzheimer's disease, respiratory and rheumatic diseases, and others. People who suffer from these diseases are much more likely to have gum disease, and people with advanced gum disease are more likely to suffer from many of these aliments.
Inflammation: A Common Thread
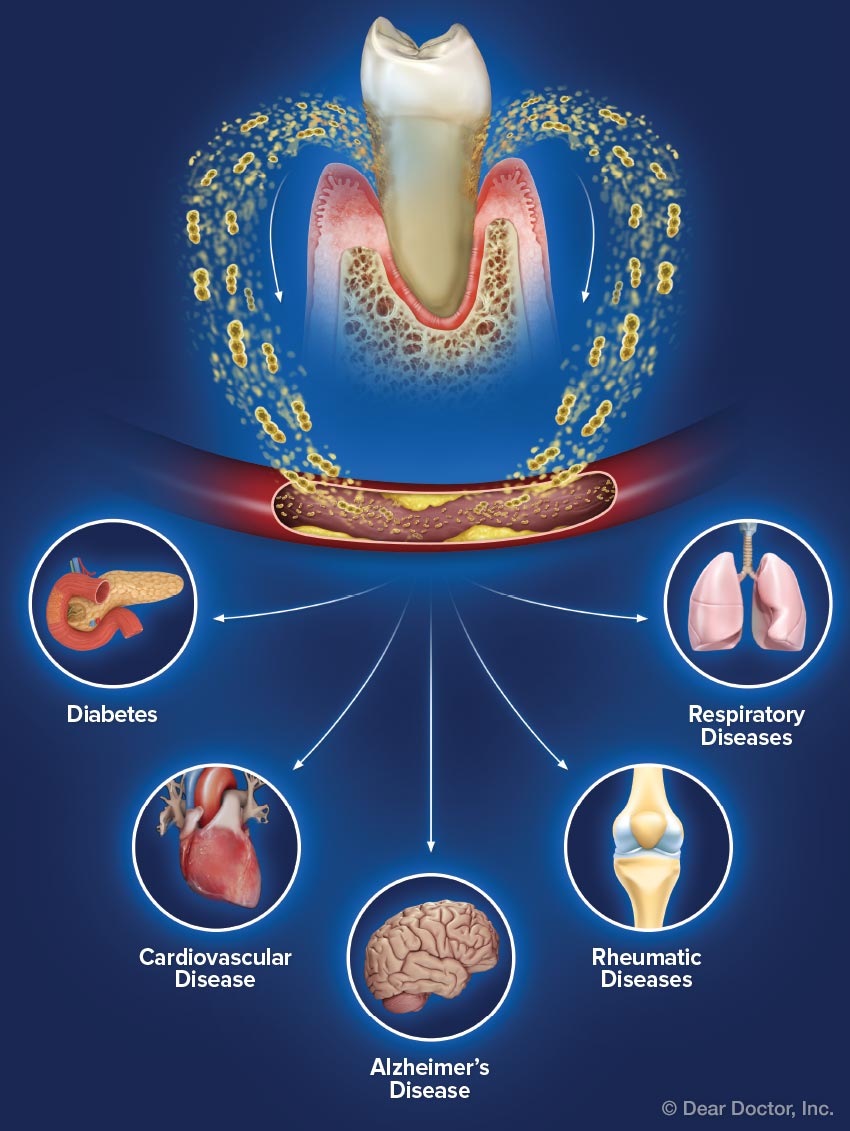
How can gum disease affect the health of other parts of the body? One connection is via harmful bacteria, which can travel between the mouth, bloodstream and lungs, potentially causing diseases in those areas. But beyond the bacteria themselves, a common thread among many systemic conditions is inflammation. While this natural process is essential to healing, too much inflammation can have negative effects.
The inflammatory response is an important part of the human immune system. An acute (abrupt) response begins soon after injury or infection: White blood cells are mobilized, releasing chemicals to fight off foreign substances; blood flow to the affected region increases, and the walls of tiny blood vessels become more porous, allowing substances to pass through more easily. The acute inflammatory response is the body's way of quickly removing harmful stimuli or microscopic invaders and beginning the healing process.
But sometimes inflammation becomes chronic, meaning that it persists over a long time, and it can adversely affect your health. Chronic inflammation may be caused by an uncontrolled infection, a foreign substance that remains in the body, or an overactive immune response.
Researchers suspect that the inflammation associated with periodontal disease is what links it with other systemic diseases. After all, gum disease is the most common chronic inflammatory disease in humans. If the body is continuously fighting a periodontal infection, the persistent immune response that is designed to promote healing can instead become an agent of tissue damage and systemic disease. Studies suggest that chronic low-level inflammation can contribute to Alzheimer's disease, Parkinson's disease, obesity, and some types of cancer.
 |
| Harmful bacteria can enter the bloodstream through the gums, causing localized and systemic inflammation.
Click to enlarge |
Systemic Diseases
A number of systemic diseases have known or suspected links to periodontal disease. Here are some of the most common ones:
Diabetes
Close to 30 million people in the U.S. have Type II diabetes, and the connection between gum disease and diabetes is one in which trouble goes both ways. Research shows that people with poorly controlled diabetes are more susceptible to gum disease and have decreased ability to fight infection. And, in turn, periodontal disease (like other infections) can make diabetes harder to control. Blood sugar is a factor linking the two diseases: A higher level of glucose in saliva feeds oral bacteria, making gum disease worse; it also makes diabetes harder to manage. Diabetes may also injure the walls of blood vessels, which interferes with the body's ability to remove waste products. Accordingly, the better you control your blood sugar, the lower your risk of gum disease; and the better you control your gum disease, the fewer ill effects of diabetes you may face.
Cardiovascular Disease
People with periodontal disease are twice as likely to have cardiovascular disease, the number one cause of death in the U.S. Research shows that gum disease makes existing heart conditions worse and increases the chance of stroke. Oral bacteria have been found in arterial plaque: hardened deposits that form on the walls of blood vessels, which can cause a dangerous constriction of blood flow. In addition, the inflammatory response triggered by periodontal disease can damage blood vessels and cause blood clots, which may block arteries and lead to heart attack and stroke. On a positive note, a 2017 study found that intensive treatment for gum disease lowered blood pressure up to 13 points.
Alzheimer's Disease
Periodontal disease has been identified as a "probable risk factor" for Alzheimer's disease, which affects 5.7 million U.S. adults. A 2017 study found that people over age 70 who had gum disease for 10 years or more were 70% more likely to get dementia than those with healthy gums. Another study found that people with Alzheimer's who also had gum disease declined more rapidly over a six-month period than those without gum disease.
Respiratory diseases
Harmful bacteria from periodontal disease can be inhaled into the lungs, causing bronchitis, emphysema and pneumonia—and chronic inflammation from periodontal disease may worsen these conditions. COPD, or chronic obstructive pulmonary disease, is the third leading cause of death in the United States. This inflammatory lung disease includes chronic bronchitis, emphysema and sometimes asthma. Although smoking is the biggest contributing factor to respiratory diseases, periodontal disease plays a role in contracting bronchitis, emphysema and pneumonia, and making COPD worse.
Rheumatic Diseases
Rheumatic diseases include many potentially debilitating conditions that can damage the joints, connective tissue and other parts of the body. These chronic, progressive inflammatory diseases make life painful for some 4 million Americans. Moderate to advanced gum disease is common in people with rheumatoid arthritis—and those who have the disease and also suffer from advanced periodontal disease tend to have more painful flare-ups. A higher incidence of gum disease and more severe gum disease are found among people with other immune-related chronic inflammatory diseases as well, including lupus and inflammatory bowel disease. Again, research points to a two-way street: Just as people with chronic, progressive inflammatory diseases may be at risk of periodontal disease, periodontitis seems to contribute to the progression of these conditions.
What You Can Do
While there is clearly a connection between gum disease and many systemic diseases, in most cases researchers cannot definitively say that gum disease causes these other diseases or that these other diseases cause gum disease. However, research points to oral health as a major signpost for overall health and a link to specific systemic diseases. Here's what you can do to improve your oral health:
- Make good dental hygiene a habit. Early-stage gum disease can usually be reversed with good oral hygiene, so brush your teeth morning and night with fluoride toothpaste, and floss once a day.
- Know common signs of gum disease. These include red, swollen, tender gums or gums that bleed with brushing and flossing. People with gum disease may notice that their gums are receding or that their teeth appear longer, feel loose or are separating from the gums.
- See your dentist. If you have gum disease or a systemic health condition, it is especially important to see your dentist at least twice a year for checkups and professional cleanings. Let your dental team know if there have been any changes to your health or medications.
- Stop smoking. Smoking—or using tobacco in any form—is one of the most significant risk factors for developing gum disease. Of course, it's also a major risk factor for many types of cancer and other diseases. So if you need one more reason to quit, gum disease could be it.
- Watch your weight. Carrying extra weight can contribute to a variety of health problems, and losing even a few pounds can have a big payoff. Weight loss is a major factor in reducing the incidence of diabetes: A large study found that the risk of diabetes decreased by 16% for every 1 kilogram (= 2.2 pounds) lost.
- Pay attention to your diet. Research also suggests that diet can have an effect on gum disease. One recent study found that an "anti-inflammatory" diet—one low in refined carbohydrates and rich in whole grains, Omega-3 fatty acids, vitamins C and D, antioxidants, and fiber—can help control gum disease. Many researchers have found that avoiding empty calories, sugary foods and drinks (including sodas and other sweetened beverages), and highly processed foods can help improve your oral—and overall—health.
- Keep your body and mind active. People who incorporate regular physical activity into their life lower their incidence of diabetes by 44% even without losing weight, according to one study—so it could help to take a short walk every day, join a gym, invest in a piece of home workout equipment…or take the stairs instead of the elevator. Equally important is taking care of your mental health. Keeping up your social life and engaging your brain with puzzles, intellectual pursuits and new experiences can help stave off mental decline.
With careful management, many systemic diseases can be well controlled—even if they can't be fully cured. Likewise, periodontal disease deserves consistent attention and proper care. Monitoring your oral health and paying attention to the early symptoms of periodontal disease can lead to better overall health, and an improved quality of life. If you have questions or concerns about periodontal disease, your dentist can be a great source of information and help.